Many patients do not know how to know that you have osteochondrosis, but at the same time they are happy to make such a diagnosis for themselves. Meanwhile, back, lower back, or neck pain can have many causes. These may be curvature of the spine, destruction of internal organs, tumors, infections, unstable vertebral body positions, etc. Therefore, you should not self-diagnose. In case of pain, seek medical attention.
There are no reliable algorithms for specific tests to identify osteochondrosis. But there are some clinical signs to suspect the disease. We'll discuss them in the material that catches your eye. At the same time, we recommend that you become familiar with the mechanisms of osteochondrosis development.
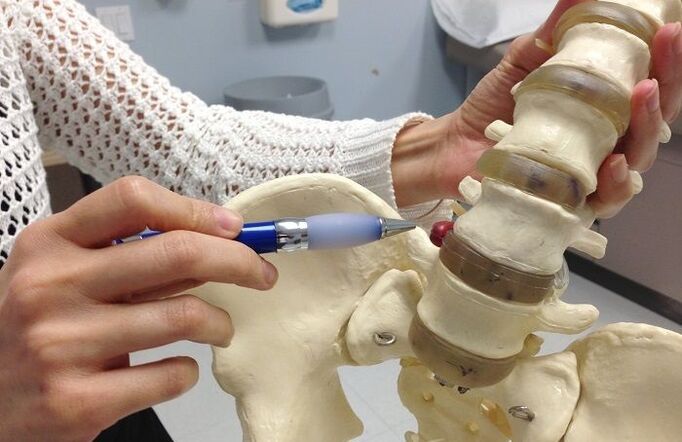
Degenerative dystrophic disease of the cartilage tissue of the intervertebral disc - this is what is scientifically known as osteochondrosis. As it develops, it can cause back pain, along with back pain, sciatica, sciatica, lumbago, and other syndromes associated with various tissue damage.
Osteochondrosis is the result of maintaining a wrong lifestyle. Contributing factors are:
- Overweight - extra depreciation and mechanical load per kilogram on the cartilage tissue of the disc;
- A sedentary lifestyle without regular exercise of the back muscles;
- Eating lots of carbohydrates, refined foods;
- wearing tight, uncomfortable clothing and shoes;
- Incorrect posture, stooping, hunched back, habit of leaning in one direction or another;
- Incorrect foot position in the form of flat feet or clubfoot;
- curvature of the spine;
- Sedentary work or strenuous physical labor;
- smoking and drinking alcoholic beverages;
- Inadequate access to clean drinking water during the day.
All of these factors slow down the microcirculation of blood in the capillary network in the thickness of the muscle tissue. It turns out that it is unable to conduct a full diffusion exchange with the cartilage tissue of the disc. They don't have their own circulatory system. This is how the mechanism of surface destruction of the annulus fibrosus, which is the outer shell of the intervertebral disc, kicks in. It forms calcium salt deposits. They prevent receiving liquids from the outside. As a result, the annulus fibrosus begins to draw fluid from the nucleus pulposus, which lies within it. This gelatinous body is responsible for maintaining the normal height and shape of the disc. Therefore, as the fluid is lost, the nucleus pulposus loses its ability to maintain the height of the disc. The second stage of development of osteochondrosis - prominence.
In the third stage, the annulus fibrosus ruptures and part of the nucleus pulposus is shed. This is a herniated disc. It compresses the surrounding soft tissues, causing inflammatory reactions, etc.
The fourth stage of osteochondrosis is the isolation of intervertebral hernias. Part of the nucleus pulposus dissociates or exits completely through the resulting rupture of the annulus fibrosus. If the hernia enters the spinal canal, its isolation requires emergency surgery. Otherwise, a person may be paralyzed for life and physically paralyzed.
As you can see, this is a very serious condition that requires prompt diagnosis. The sooner complex treatment is started, the higher the chance of fully restoring the integrity of the disc and its function.
When the first signs of osteochondrosis appear, you can make an appointment with a spondylologist or neurologist. Doctors will perform examinations and manual examinations. They will make an accurate diagnosis and recommend necessary additional tests. After an accurate diagnosis is made, you will be offered a course of treatment.
How to identify cervical osteochondrosis
How to know you have cervical osteochondrosis, not myositis, and what to do next? Before identifying cervical osteochondrosis, you will need to collect medical records:
- when pain occurs;
- what kind of behavior will cause them to appear;
- How long ago was the first seizure;
- whether there are any other clinical symptoms;
- how sleep and workplace are organized;
- any bad habits
- Work location and occupation.
How to understand cervical osteochondrosis based on all this information? First of all, it is important to know that degenerative degenerative disease of the intervertebral disc manifests itself only in the initial stages in the form of pain, stiffness of movement, and muscle strain in the neck and collar area. Then, signs of tension headaches, dizziness, hearing and vision disturbances, increased fatigue, and decreased mental performance were added to the list.
A distinguishing feature of cervical osteochondrosis is that the worsening of symptoms begins at the end of the workday. In most cases, the occupational activities of patients are associated with prolonged static tension in the muscles of the neck and collar area. On examination, the spinous processes of the vertebrae were painful to palpation, and the pain was exacerbated by muscle hypertension and attempts to turn the head.
Before identifying osteochondrosis in the neck area, doctors recommend that patients have an x-ray. It shows reduced space between the vertebral bodies. This indicates that protrusions are developing. With the help of X-ray images, an experienced spondylologist will be able to rule out instability of the vertebral body position, subluxation, posterior slip, anterior slip, intervertebral joint destruction and many other serious pathologies. If this test is not enough, then an MRI or CT scan is recommended. If you suspect the development of posterior vertebral artery syndrome, an ultrasound scan of the blood vessels in the neck and head is recommended.
How to Identify Thoracic Osteochondrosis
Before identifying thoracic vertebral osteochondrosis, the possibility of pathological changes in internal organs such as the heart, coronary circulatory system, lungs, pleura, and bronchi must be excluded. Consider how to identify osteochondrosis in the chest area:
- The most important diagnostic technique is palpation, if the pain is determined only by the spinous processes of the vertebrae and the area of the paravertebral muscles, degenerative destruction of the cartilage tissue of the intervertebral disc is not excluded;
- Limited movement, any turning and tilting of the body will increase pain;
- The onset of pain is caused by physical exertion, hypothermia, or psychological stressors;
- Deep breathing will not make the pain worse.
Knowing how to understand cardiac or osteochondrosis is important because acute chest pain is often a precursor to myocardial infarction. In this case, immediate cardiac care should be provided to the patient.
So if you experience anxiety, panic and fear of death during a pain attack, there is a 90% chance of a heart attack and you need to call an ambulance urgently. If you have a tonometer, then you'll need to measure your blood pressure and count your pulse. Unstable angina episodes, with possible transition to myocardial infarction, should also be suspected when the pulse slows to bradycardia (less than 50 beats per minute) and blood pressure rises 20-40 mm Hg above normal for age.
You shouldn't be looking for information on how to understand heartache or osteochondrosis, it's more productive to seek medical help. Even the most common electrocardiogram, taken in a hospital emergency department, can show what's causing the pain syndrome: the heart or the spine. Independently, you can only rely on sensation on palpation. Usually, palpation of the spinous processes of the vertebrae does not produce any unpleasant sensations due to myocardial damage. At the same time, the clinical symptoms of osteochondrosis include shortness of breath, shortness of breath, pale skin, cold sweat and sticky skin, cyanosis of the nasolabial fold, and severe muscle weakness.
How to Identify Lumbar Osteochondrosis
The question of how to understand osteochondrosis of the lumbar spine can cause severe pain is acute. In addition, with the failure of some paired root nerves as well as plexuses, clinical symptoms similar to those of gastrointestinal and urinary disorders occur. These are constipation, diarrhea, frequent urination, etc.
How to know your back osteochondrosis is causing pain and all other clinical symptoms:
- body temperature does not rise;
- no nausea and vomiting;
- The tongue does not have a white or yellow coating;
- When urinating, the color of the urine is the same as normal;
- No tenesmus and other pain when emptying the bowel;
- There is no mixture of blood or mucus in the stool.
To rule out renal pathology, Pasternatsky's symptoms were tested. The patient stands up straight with his back to the doctor. The doctor gently taps the edge of the lower costal arch with the edge of the palm. If pain occurs, low back pain is most likely related to damage to the kidneys and ureters.
How to recognize lumbar osteochondrosis by indirect signs:
- sharp increase in pain with any movement;
- The condition begins to worsen after severe physical exertion, weight lifting, hypothermia, or overheating;
- Feeling of stiffness in movement, usually associated with muscle weakness;
- Extreme muscle tension in the lower back, pain on palpation;
- Pain can travel along the paths of large nerves, for example, the groin area, anterior abdominal wall, lower extremities;
- At rest, the pain syndrome goes away quickly.
When characteristic symptoms of osteochondrosis develop, it is important to contact a neurologist or chiropractor as soon as possible. Only an experienced doctor can rule out vertebral body displacement, herniated discs, spinal stenosis, and other dangerous conditions that require immediate medical attention.
Pain caused by osteochondrosis
We figured out how to understand that pain is caused by osteochondrosis. Now, this is important information. You need to know how to do it right and how to get rid of this disease.
Degenerative disease of the disc cartilage tissue does not go away on its own. This is due to many factors. First, calcification occurs on the surface of the annulus fibrosus, thus losing the ability to absorb fluids secreted by working muscles. Second, secondary contractions of ligaments and tendons occur during the reduction in disc height. It is not possible to restore the height of the intervertebral space required to correct the disc on its own.













































